Eczema



What is Atopic Dermatitis?
How prevalent is AD in children?
What are the clinical features of Atopic Dermatitis?
Rashes
Red to brownish-gray colored patches
Itching, which may be severe, especially at night
Small, raised bumps, which may leak fluid and crust over when scratched
Thickened, cracked or scaly skin
Raw, sensitive skin from scratching
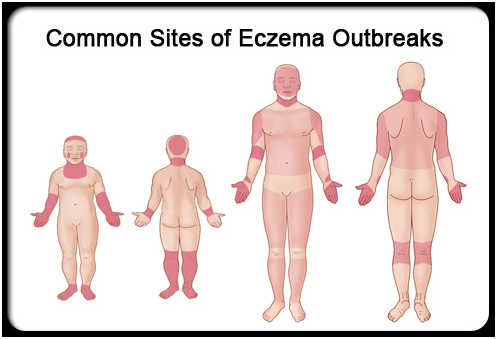
Distribution of rashes
Course of the disease
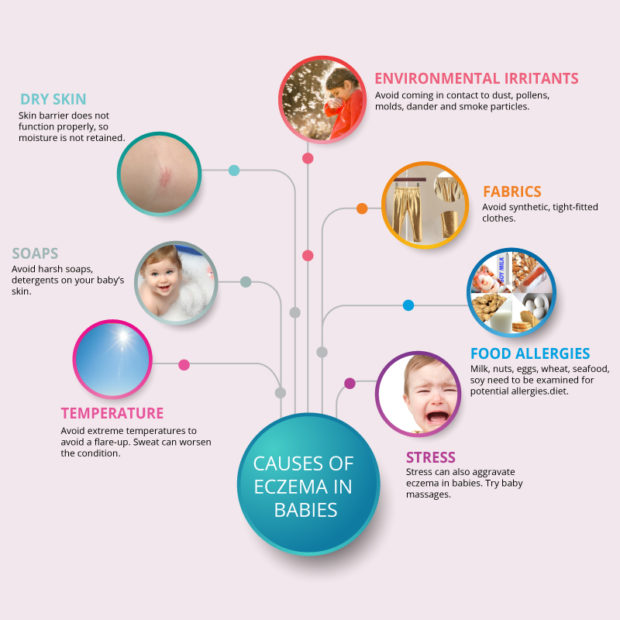
What are the causes of Eczema?
Is this disease has genetic links?
What are the types of Eczema (Dermatitis) ?
Allergic contact eczema (dermatitis)
A red, itchy, weepy reaction where the skin has come into contact with a substance that the immune system recognizes as foreign, such as poison ivy or certain preservatives in creams and lotions.
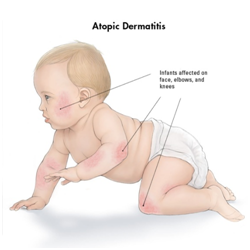
Atopic dermatitis
A chronic skin disease characterized by itchy, inflamed skin.
Contact eczema
A localized reaction that includes redness, itching, and burning where the skin has come into contact with an allergen (an allergy-causing substance) or with an irritant such as an acid, a cleaning agent, or other chemical.
Dyshidrotic eczema
Irritation of the skin on the palms of the hands and soles of the feet characterized by clear, deep blisters that itch and burn.
Neurodermatitis.
Scaly patches of the skin on the head, lower legs, wrists, or forearms caused by a localized itch (such as an insect bite) that become intensely irritated when scratched.
Nummular eczema
Coin-shaped patches of irritated skin—most common on the arms, back, buttocks, and lower legs—that may be crusted, scaling, and extremely itchy.
Seborrheic eczema
Yellowish, oily, scaly
Stasis dermatitis
A skin irritation on the lower legs, generally related to circulatory problems
What are the Factors that worsen Atopic Dermatitis?
Other factors that can worsen signs and symptoms of atopic dermatitis include:
1
Dry skin
3
Stress
5
Rapid changes in temperature
7
Solvents, cleaners, soaps or detergents
9
Dust or sand
11
Living in cities where pollution is high

2
Long, hot baths or showers
4
Sweating
6
Low humidity
8
Wool or man-made fabrics or clothing
10
Cigarette smoke
12
Certain foods, such as eggs, milk, fish, soy or wheat

When to see an Allergist?
See your Allergist if:
You’re so uncomfortable that you’re losing sleep or are distracted from your daily routines
Your skin is painful
You suspect your skin is infected
You’ve tried self-care steps without success
If you suspect your child has Atopic Dermatitis or you notice the above signs and symptoms, see your child’s doctor.
Early, effective treatment helps keep atopic dermatitis from worsening. The more severe it becomes, the more difficult it is to control.
Complications of Atopic Dermatitis (Eczema) include:



Neurodermatitis
Skin infections






Eye complications
How atopic dermatitis is treated?
Avoidance of irritant & specific triggersAvoidance of allergen
Avoid swimming in chemically treated pools
Avoid extreme temperature and humidity
Avoid extreme temperature and humidity
Avoid occlusive clothing
Food allergens: milk, egg, peanuts, soy, wheat, and fish. Avoid implicated food completely
Repair and maintenance of skin barrier
Moisturizers-emollient + hydration therapy restores and preserve the skin barrier.
Interruption of itch scratch cycle-systemic antihistamines and anxiolytics are helpful
Reduction of inflammation
THE ATOPIC MARCH
Severity of AD and risk of development of asthma
1
Normal subjects (without AD) 8%
2
Mild AD 20%
3
Severe 70%





