Food Allergy


What is Food Allergy?
Food Allergy is an abnormal response of immune system triggered by food. Most of the reactions are IgE mediated. It can involve skin, gastrointestinal tract, respiratory tract and in severe cases cardiovascular. Manifestations may happen immediately post ingestion, though in some cases it may take hours to days.
It can be seasonal, year round or occupationa
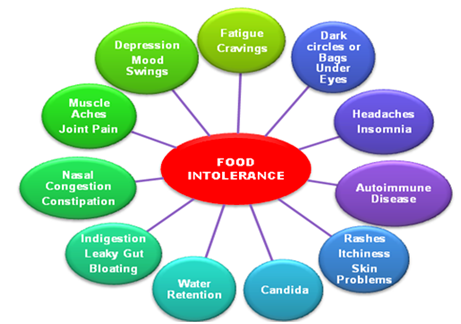
What is Food Intolerance?
Food intolerance or non-allergic food hypersensitivity is a term used widely for varied physiological responses associated with a particular food, or compound found in a range of foods. Food intolerance is a detrimental reaction, often delayed, to a food, beverage, food additive, or compound found in foods that produces symptoms in one or more body organs and systems, but it is not a true food allergy. A true food allergy requires the presence of immune mechanisms (as for instance Immunoglobin E – IgE antibodies) against the food, and food intolerance does not.


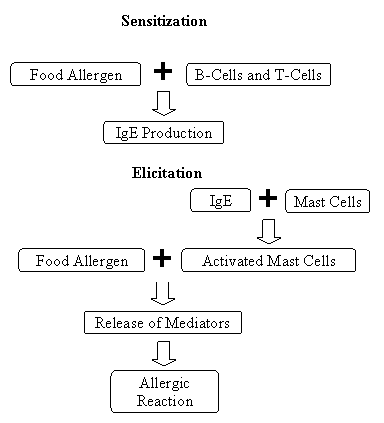


How Food Allergies Work?
Food allergies involve two features of the human immune response. One is the production of immunoglobulin E (IgE), a type of protein called an antibody that circulates through the blood. The other is the mast cell, a specific cell that occurs in all body tissues but is especially common in areas of the body that are typical sites of allergic reactions, including the nose and throat, lungs, skin, and gastrointestinal tract.
The ability of a given individual to form IgE against something as benign as food is an inherited predisposition. Generally, such people come from families in which allergies are common — not necessarily food allergies but perhaps hay fever, asthma, or hives. Someone with two allergic parents is more likely to develop food allergies than someone with one allergic parent.
Before an allergic reaction can occur, a person who is predisposed to form IgE to foods first has to be exposed to the food. As this food is digested, it triggers certain cells to produce specific IgE in large amounts. The IgE is then released and attaches to the surface of mast cells. The next time the person eats that food, it interacts with specific IgE on the surface of the mast cells and triggers the cells to release chemicals such as histamine. Depending upon the tissue in which they are released, these chemicals will cause a person to have various food allergy symptoms. If the mast cells release chemicals in the ears, nose, and throat, a person may feel an itching in the mouth and may have trouble breathing or swallowing. If the affected mast cells are in the gastrointestinal tract, the person may have abdominal pain, vomiting, or diarrhoea. The chemicals released by skin mast cells, in contrast, can prompt hives.
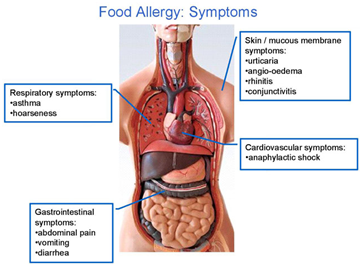
Symptoms
An allergic reaction to food can affect the skin, the gastrointestinal tract, the respiratory tract, and, in the most serious cases, the cardiovascular system. Reactions can range from mild to severe, including the potentially life-threatening condition known as anaphylaxis. Symptoms typically appear within minutes to several hours after eating the food to which you are allergic. Keep in mind that children may communicate their symptoms in a different manner than adults.


Mild symptoms may include one or more of the following:
Hives (reddish, swollen, itchy areas on the skin)
Eczema (a persistent dry, itchy rash)
Redness of the skin or around the eyes
Itchy mouth or ear canal
Nausea or vomiting
Diarrhea
Stomach pain
Nasal congestion or a runny nose
Sneezing
Slight, dry cough
Odd taste in mouth
Uterine contractions
Severe symptoms may include one or more of the following:
Obstructive swelling of the lips, tongue, and/or throat
Trouble swallowing
Shortness of breath or wheezing
Turning blue
Drop in blood pressure (feeling faint, confused, weak, passing out)
Loss of consciousness
Chest pain
A weak or “thread” pulse
Sense of “impending doom”
Severe symptoms, alone or in combination with milder symptoms, may be signs of anaphylaxis and requires immediate treatment.
How a Child Might Describe a Reaction
Children have unique ways of describing their experiences and perceptions, and allergic reactions are no exception. Precious time is lost when adults do not immediately recognize that a reaction is occurring or don’t understand what a child is telling them.
Some children, especially very young ones, put their hands in their mouths or pull or scratch at their tongues in response to a reaction. Also, children’s voices may change (e.g., become hoarse or squeaky), and they may slur their words.
The following are examples of the words a child might use to describe a reaction:
“This food is too spicy.”
“My tongue is hot [or burning].”
“It feels like something’s poking my tongue.”
“My tongue [or mouth] is tingling [or burning].”
“My tongue [or mouth] itches.”
“It [my tongue] feels like there is hair on it.”
“My mouth feels funny.”
“There’s a frog in my throat.”
“There’s something stuck in my throat.”
“My tongue feels full [or heavy].”
“My lips feel tight.”
“It feels like there are bugs in there.” (to describe itchy ears)
“It [my throat] feels thick.”
“It feels like a bump is on the back of my tongue [throat].”
Severe symptoms, alone or in combination with milder symptoms, may be signs of anaphylaxis and requires immediate treatment.



Food Allergen
Although nearly any food is capable of causing an allergic reaction, only eight foods account for 90 percent of all food-allergic reactions . These foods are:
1
Peanuts
2
milk
3
wheat
4
shell

5
treenuts
6
egg
7
soy
8
fish

Do not diagnose a food allergy on your own. Self-diagnosis can lead to unnecessary dietary restrictions and inadequate nutrition, especially in children. Visit your Allergist for accurate diagnosis. Additionally, some people think they are allergic to a food when they actually have another type of food disorder, and treatment may differ.
How a Child Might Describe a Reaction
Diagnosis
The first step an allergist will take to diagnose a food allergy is a thorough medical history. The allergist will ask questions to determine if food allergy may be causing your symptoms and to identify the culprit food(s), and will then perform a physical exam
Next, the allergist may conduct tests to help identify a food allergy. While these tests alone do not always provide clear-cut answers, the allergist will combine your test results with the information given in your medical history to provide a diagnosis. These tests may include:
1
Skin prick test
2
Oral food challenge

3
Blood test
4
Trial elimination diet

These tests are all proven diagnostic methods. Depending on your medical history and initial test results, you may have to take more than one test before receiving your diagnosis.
Treatment
| Type 1 | Type 2 | |
|---|---|---|
| Sex F/M | 2.5 F: 1 M | 1F:1M |
| Age yr | 15-55 | - |
| Atopy | Yes | No |
| Food intolerance | Yes | No |
| Psychological factors | Yes | No |
| Morbidity | High | - |
| Mortality | - | High |




